62 yr old male came to opd for dialysis
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
Khushi Tulsyan
Roll no. 75
A 62 yr old male farmer by occupation presented to opd for dialysis.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 1 month back.Then he has shortness of breath while climbing Upstairs ( grade 2) Then he had decreased appetite. Then he started having shortness of breath since 10 days back even while talking . He had a decrease in his appetite since 10 days and low grade continuous fever so he visited local hospital where in routine examination he was found to be having raised levels of serum creatinine and was advised for a dialysis. He was also diagnosed of having areas of Cystic Bronchestiasis (with fibrotic bands and adjacent pleural thickening in right upper lobe and fibroelastic bands in left upper lobe and right middle lobe) in that hospital.He stayed in the hospital for 4 days and then he left the hospital against medical advice.
He then presented to our op for Dialysis.
He had lost 5-6 kgs in the last 1 month.
DURING STAY IN HOSPITAL-
He had an 1-2 episodes / day of vomiting which was yellowish in colour, non projectile, non bililus, watery, foul smelling with no sputum.
PAST HISTORY-
He is a known hypertensive and diabetic from 5 yrs ( which was known during a pre op examination)
He is not a known case of aastha, leprosy, CAD, CKD, epilepsy.
For hypertension he is known to be taking Atenolol and for diabetes metformin 1 tab in morning daily.
He had a right leg operation for facture 5 yrs back after a sudden fall
He doesn't work after that operation and uses a stick to walk.
PERSONAL HISTORY-
He has a mixed diet, with decreased appetite since 20 days with a regular bowel and bladder movements . He has no allergies.
He is known to be smoking since years 2times / day.
FAMILY HISTORY-
No significant family history.
GENERAL EXAMINATION:
Patient is examined under well lit room and adequate ventilation with his consent taken
Patient is conscious , coherent and cooperative well orientated to time, space and person. He is moderately built and nourished.
Pallor is present.
No icterus, edema, lymphadenopathy, clubbing, Cyanosis.
VITALS-
Temp - afebrile
BP - 110/70
Pulse - 76 bpm
Resp rate - 15 cpm
Sp O2 - 97 %
SYSTEMIC EXAMINATION-
CVS -
S1, S2 heard
ABDOMEN-
Scaphoid shape
No tenderness
No palpable masses
Bowel sounds present
CNS-
No focal neurological defecits.
RESPIRATORY SYSTEM-
No dyspnea
On Inspection-
Shape of chest - barrel shaped bilateral symmetrical
Scoliosis is present.
Righ sided upper lobe area of lung was depressed.
On Palpation-
Trachea - central
On Percussion-
On Ascultation-
NVBS
No wheeze is heard
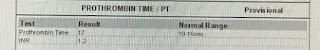
PROVISIONAL DIAGNOSIS-
Chronic kidney disease secondady to diabetic nephropathy
Cystic Bronchestiasis
PLAN OF CARE-
Lasix
Pantaprazole
Zofer









Comments
Post a Comment