60 year old male came to gm OPD with chift COMPLAINTS of pyrexia
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
Case Report-
A 60yr old female resident of Narketpally agriculture labourer by occupation came to GM OPD with
CHIEF COMPLAINTS
Fever since 4 days
Decreased micurition since 4 days
History of Presenting Illness
Patient was apparently asymptomatic then she developed high grade fever 4 days back intermittent in nature not associated with cold cough and no burning micurition but decreased micurition was seen.
5 years ago patient had selling at sacral region which increased progressively in size (not measured),no disturbance in power and tone of muscles and bowel and bladder were regular
2 years back patient patient developed tingling and numbness of upper 2 limbs and lower 2 limbs, medications was used (drug -unknown,dose-unknown) and upon using medication it did not subscide.
Weakness of limbs was progressive and tingling sensation was progressive and had burning sensation.
Patient was unable to walk without support since 6 months and complete bed ridden since 3 months
6 months ago patient developed pedel oedema from ankle to thigh region and due to this patient sleep cycle was altered.
On investigation it was concluded of compressive myelopathy where surgical laminectomy was done
Post surgery patient was feeling better and the symptoms of tingling and numbness reduced
Patient was not able to lift hands till 1 wk of post surgery.
Past history
No similar complaints in the past.
Treatment history
Laminectomy done 6 months ago
Personal history
Diet:- mixed
Appetite - decreased
Sleep:- not adequate
Bowel and bladder:- decreased urinary output and constipation
Addictions:- NIL
Family history
No significant family history
Obstetric history
G4 P3 A1 L3
Delivered through FTND
Allergic history
No known allergies to drugs and other foods
General examination
Patient is conscious coherent and cooperative.
Weakly built and weakly nourished
Tempurature-98 c
Pulse rate -82 bpm
Respiratory rate- 15cycles per min
BP -130/80 mmhg
CNS memory intact
Pallor present
Icterus no
Clubbing no
Lymphedenopathy-No
Edema No
Cyanosis No
Systemic examination
CVS- S1 and S2 heard no murmurs
Respiratory system
Bilateral aur entry present
Per abdomen
Abdominal distention seen
CNS
FINGER NOSE TEST -No coordination
Provisional diagnosis
Pyrexia with suspection of UTI
Reflexes
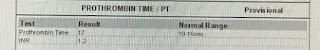
Investigation
Pallor-
CLINICAL DIAGNOSIS
Pyrexia secondary to UTI
TREATMENT
IVF NS @100ML/HR
inj.neomol iv/sos
(D2 )Tab nitrofurantoin 100mg po/bd
Syp. POTCHLOR 15ml/po/Tid
monitor vitals



















Comments
Post a Comment